The Sound Cat Veterinary Hospital
Feline
Hyperthyroidism
Feline Radioactive Iodine is a treatment that is offered at The Sound Cat Veterinary Hospital for cats that have been diagnosed with hyperthyroidism.
What is Feline Hyperthyroidism?
The thyroid glands in the cat have paired glands located midway down the neck on either side of the trachea. Rarely thyroid tissue is also present inside the chest or other parts of the body. This extra tissue is called ectopic tissue. The thyroid gland produces a hormone (called T4 or tetraiodothyronine) which when changed into the active form inside the cells of the body (called T3 or triiodothyronine) controls the rate of metabolism. In other words, this hormone controls how fast and how hard each cell works. The hormone circulates in two forms. The most commonly measured form is the bound T4 (often called the total T4). This form is bound to the plasma protein albumin. The other form is the free or unbound T4. The free T4 is the form that is biologically available to the cells of the body. Hyperthyroidism results when a population of thyroid cells begins secreting the hormone in excessive quantity. Feline hyperthyroidism was first recognized in 1979. The disease has increased in prevalence over the decades to become the most common endocrine disorder in the cat. It is estimated that as each year passes, the risk of a cat becoming hyperthyroid increases so that at age 10, there is a 30% chance of developing the disease.
The disease exists in two forms. The most common is a benign enlargement of one or both thyroid glands in what is called adenomatous hyperplasia or a benign adenoma (98%). Rarely a cat will develop spontaneous cancer called a thyroid adenocarcinoma (2%).
The cause of the disease is elusive and many theories are proposed. Risk factors include the consumption of canned food, especially the smaller “pop-top” cans, and other environmental factors such as fire retardants in carpets, upholstered furniture, and bedding. Cats have a poor ability to eliminate many chemicals from their bodies because, unlike other mammals, they lack the ability to conjugate these chemicals in a process called glucuronidation, and thus excrete the chemicals. Cumulative exposure to certain known “goitrogens” is implicated in causing the transformation of the thyroid cells. A population of cells begins working autonomously, without regulatory influence from the brain and pituitary. These cells form nodules and continue to grow and manufacture increasing amounts of hormones over time. Genetic factors have also been implicated. To date, the precise etiology is unclear.
Clinical signs in your cat are the result of “run-away” metabolism and include:
- Cardiomyopathy (heart disease)
- Hypertension (high blood pressure)
- Gastrointestinal disorders (vomiting, diarrhea)
- Dermatopathy (skin disorders, hair loss)
- Osteoporosis (loss of bone density)
- Renal disease (kidney disease)
- Behavior changes (aggression, depression, or apathy)
- Inappropriate elimination of excessive thirst and urination
The increased metabolism is similar to the effects of certain diet supplements in humans that cause weight loss but also increase heart rate. Hyperthyroid cats’ heart rate often reaches 250 – 300 beats per minute. The heart walls will thicken and the result is a decreased volume in the chambers (hypertrophic cardiomyopathy) and the development of heart murmurs. This can be life-threatening. Another circulatory problems are high blood pressure, which alone or in concert with the thyroid hormone will slowly damage the kidney. Hypertension can also lead to stroke and retinal detachment. If left untreated these changes may become irreversible and the disease is eventually fatal.
How is Hyperthyroidism Diagnosed?
A thorough physical examination once yearly (or semi-annually for cats over 10 years of age) may alert your vet to subtle changes in your cat. Annual screening with blood work, blood pressure measurement, and palpation of the thyroid glands are essential. It is important to diagnose the disease before the clinical signs become apparent. Often hyperthyroidism is detected on routine geriatric screening or pre-dental blood work.
In addition to a complete blood count and serum chemistry, the screening will include a total T4. If there is still doubt that the cat is hyperthyroid, a free T4 (free T4 by dialysis) will be requested. Occasionally there are cats whose total T4 remains in a “gray zone” while the free T4 is significantly elevated.
It is impossible to differentiate between the benign and malignant forms without biopsy. The malignant form typically affects only one of the glands and grows aggressively resulting in high values for the T4 and free T4.
What are the treatment options?
Medical Management
Conventional medical treatment consists of twice-daily administration of an anti-thyroid drug called methimazole (Tapazole). This drug does not kill the abnormal cells or cure the disease. It works by blocking the incorporation of iodine into the thyroid hormone during its manufacture inside the thyroid cell. The gland therefore can continue to grow. Another disturbing finding is that while a cat’s T4 may return to normal on Tapazole, the effects on the heart are not reversed and many cats go on to develop thyrotoxic cardiomyopathy. The drug must be monitored every 2 to 3 months with blood work for the following reasons: 1. Tapazole does not arrest the growth of the gland; the T4 levels must be checked to ensure the dose of the drug is adequate, and 2. Tapazole can cause bone marrow suppression, which in some cases is irreversible, and 3. Tapazole can cause hepatotoxicity (liver toxicity). Other side effects of the drug include gastrointestinal distress, lethargy, facial excoriation and pruritis, and other hematological abnormalities.
Tapazole therapy is often used short-term as a trial prior to the radioactive iodine therapy to evaluate the effects of “slowing down” metabolism on other organ systems when pre-existing kidney and heart disease is suspected. Medical management with Tapazole may be the treatment of choice in cats with concurrent life-threatening diseases whose life expectance is short and the cost of other therapy is prohibitive.
The average cost of medical management for hyperthyroidism is $600 – $900. per year.
Surgical Management
Surgical removal of one or both thyroid glands had been popular until the introduction of affordable nuclear medicine. When only one lobe is removed, the disease recurs in 70 – 90% of the cases within 2 years. If both lobes are removed, the cat will likely require hormone replacement. Surgical removal of the cervical thyroids (tissue in the neck) may not address the presence of ectopic thyroid tissue in other parts of the body, usually in the chest. The inherent risks of the surgery include anesthesia for a geriatric patient with varying degrees of heart disease and the risk of damaging the parathyroid glands that share capsular tissue with the thyroid. Damage to both parathyroid glands results in abnormal and life-threatening calcium and phosphorus imbalances. Finally, even in the best of surgeries, a fair number of the cats become hyperthyroid again within 3 years due to regrowth at the surgical site or hyperplasia of ectopic tissue. Surgical therapy may be indicated when immediate results are necessitated by imminent heart failure.
If surgery is necessary, many of the disadvantages of surgical thyroidectomy have been minimized by the use of state-of-the-art anesthesia and monitoring equipment, and the use of the surgical microscope and laser. The surgical microscope allows the surgeon to easily visualize the parathyroid gland and its blood supply and other crucial structures like the fine nerves to the larynx. The procedure is also laser-assisted which results in a bloodless surgical field and virtually complete removal of the thyroid tissue) minimizing recurrence). Laser surgery also results in less swelling and less pain for the patient. While this surgical procedure has inherent risks, they are minimized with the use of sevoflurane anesthesia, state-of-the-art surgical monitors, and blood gas analysis. Typically the cats go home the day after surgery following a blood calcium level to confirm that the parathyroid gland is functional. The cost for the surgery is around $800. This includes a pre-operative consult and examination, chest radiographs, electrocardiogram, cardiac and abdominal ultrasound, and a post-operative calcium level.
Radioactive iodine therapy
Radioactive iodine therapy is now considered the treatment of choice for feline hyperthyroidism. The therapy is 96% effective with one treatment. Rarely a cat may require a second dose. This may be necessary if the cat is eating a diet high in iodine or is taking supplements that interfere with the absorption of iodine or if the cat has a radio-resistant adenocarcinoma. The cure rate after the second dose in these individuals is virtually 100%. There are no serious direct side effects and the therapy is painless and does not require anesthesia. When a cat is administered an average dose, the hospital stay is 3 days. If larger doses are given, the stay may be up to 5 days. Within 2-4 weeks, your cat’s thyroid function will return to normal.
How do we identify a good candidate for therapy?
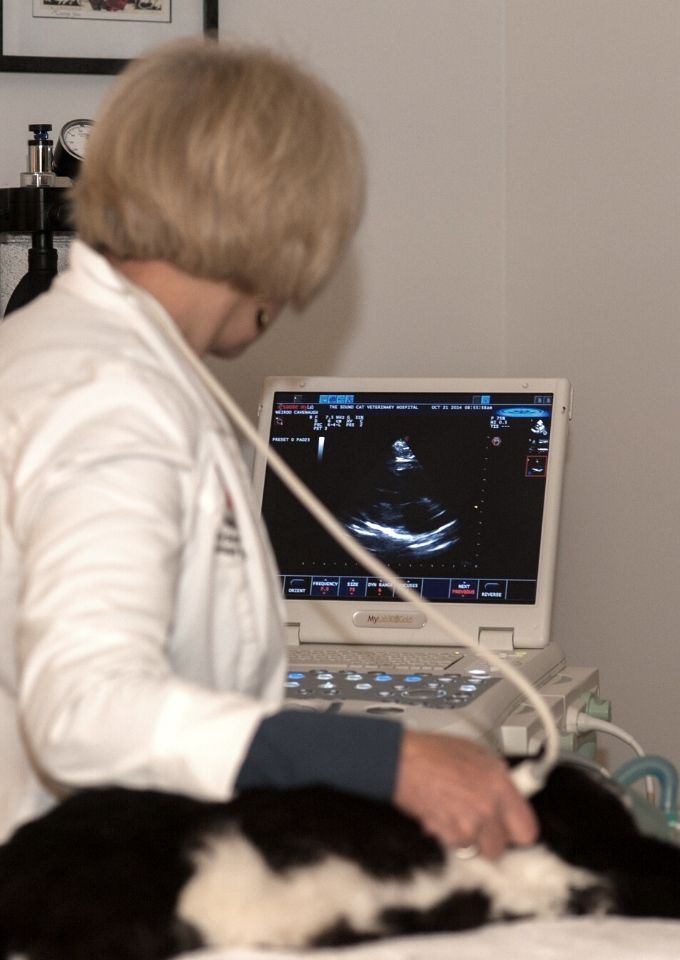
Age is not a factor. We have treated cats from 3 years of age to 20 years of age. The cat must be in reasonably good health, that is, have no underlying disease that will be adversely affected when the metabolism and blood pressure returns to normal. Your vet will provide us with recent chemistries, T4 values, complete blood count, and urinalysis. We will examine the cat, obtain indirect blood pressure, an electrocardiogram, chest and abdominal radiographs, and perform cardiac ultrasound (echocardiogram) and abdominal ultrasound. If your vet has not provided us with adequate blood work, we can obtain it at the time of examination. These diagnostic tests will give us a great “window” into your cat’s overall health. If we find any worrisome changes, we will discuss them immediately with you and your veterinarian. In rare cases, it may be necessary to stage the therapy with smaller doses to allow for compensation by compromised systems. Once the cat has been examined, we calculate the dose of radioactive iodine to be administered and place the order. The unit dose is delivered from a local nuclear pharmacy within an hour or two and your cat receives his therapy solution on the same day as admission. We encourage people who have traveled from out of town to wait while we perform the diagnostics.
How does the therapy work?
The dose of 131 iodine is supplied in 0.2ml volume in an insulin syringe and is administered subcutaneously between the shoulders. Your cat will not feel the injection. The 131 iodine is absorbed immediately into the circulation where it saturates the abnormal thyroid cells for about 12 hours. Normal thyroid cells do not absorb the iodine because they are atrophied. Since the thyroid is the only tissue that utilizes iodine, only the active (abnormal) thyroid cells will absorb the iodine. Over the next 36 – 48 hours, the iodine that has not been absorbed by the thyroid cells will be excreted by the cat primarily into the urine. This is why they must remain in our care for this period. Within days the abnormal cells will be destroyed by the intracellular beta radiation and the T4 levels will start to decline. When the T4 levels drop, the atrophied normal tissue is activated and normal amounts of thyroid hormone are produced. It is rare that hormone supplementation is necessary after the therapy. When your cat is released to go home, the radiation is concentrated in the thyroid tissue and is at a very safe level. There is no collateral tissue damage with this therapy.
What side effects may I see?
While there are no direct side effects, we sometimes see the cat become quiet, almost lethargic and eat less during a transient period before the atrophied normal tissue begins to make hormones. We rarely see a cat develop a “sore throat” 3-7 days after the therapy. This is the result of the mildly inflammatory reaction in the thyroid while the body is absorbing the dying thyroid cells. We call this radiation thyroiditis. It is usually self-limiting with anti-inflammatory medication. With thyroiditis, the cat appears hungry but may have difficulty swallowing. Finally, rarely do we see a change in vocalization (hoarse meow) that is usually transient.
Why do I need to stop the thyroid drug?
You must stop the methimazole 5 -7 days prior to the therapy because it will interfere with the uptake of the 131 iodine. If your cat will become unstable off the drug, we will accept a shorter time but that must be discussed with Dr. Williams. Normally, recurrence of mild symptoms can be controlled during that week.
Do other drugs interfere?
Certain drugs, foods, and herbal supplements will interfere with the therapy. Please consult Dr. Williams for these drugs. Do NOT discontinue antibiotics or heart medication. The cat may eat normally on the day of the therapy.
May I visit my cat?
State and federal regulations prohibit us from allowing you to visit during the quarantine period. Once admitted, your cat cannot be discharged until the radiation is at a safe exposure level. While the total amount of radiation emission is small, our concern is that we minimize your total lifetime cumulative radiation exposure. You may send along a small toy oquarantiner article from home but you will not get it back after the treatment since the article will be placed in storage for isotope decay.
Where is my cat during these three days?
Our nuclear medicine ward is furnished with bright comfortable large cat condos. The room is climate controlled and isolated from the rest of the hospital. Classical music is played for enrichment. Their litter boxes are kept clean at all times and they are given comfortable bedding. Their diet is maintained as close to home as possible. You may call daily for updates.
What can I expect on discharge?
You will be given a discharge appointment at which time Dr. Williams will discuss your cat’s case and explain the post-treatment precautions that you must observe for 2 weeks following discharge.
Is this therapy dangerous to me and my other pets?
The amount of radiation remaining in your cat’s thyroids on discharge is very low. Most cats receive between 2 and 4 mCi of therapy solution containing radioactive iodine. By comparison, humans with hyperthyroidism receive 30 – 150 mCi of radioactive iodine and go home the same day of the treatment with far fewer restrictions. Cross-country flights on commercial airliners expose us to about the same amount of radiation that your cat will emit. The difference is that we control where we eliminate and sometimes the cats do not eliminate where they should. It is safe to allow your other pets to share the litter box and food bowls as well. Our pets have a shorter life span and do not have cumulative exposure to environmental and occupational radiation, as do we in the course of our life.
Why does my cat need an echocardiogram and ultrasound?
The package includes additional diagnostic procedures (echocardiogram, abdominal ultrasound, and radiographs. These additional diagnostic tests ensure the safety of your cat and the efficacy of the therapy. These diagnostics, in many cases, have detected other diseases or conditions that affect the outcome of the therapy or may present a clinical problem in the near future.
What follow up does my cat need?
Each case is unique and in some cases, Dr. Williams would like the cat seen in 2 weeks or sooner. Most cases will have their first follow-up at 30 days post-therapy. Your vet will receive a summary of the diagnostic findings and the recommendations for tests that Dr. Williams would like to have performed at the examination. Your primary care veterinarian will then forward the results to Dr. Williams.
If your cat experiences any complications within the first few months following the therapy, Dr. Williams would be happy to consult with you and your veterinarian.